No matter which IOL is used the surgeon will need to select the appropriate power of IOL (much like an eyeglass prescription) to provide the patient with the desired refractive outcome. Traditionally doctors use preoperative measurements including corneal curvature, axial length, and white to white measurements to estimate the required power of the IOL.
These traditional methods include several formulas including Hagis, Hoffer Q, Holladay 1, Holladay 2, and SRK/T to name a few. Refractive results using traditional power calculation formulas leave patients within 0.5D of target (Correlates to 20/25 when targeted for distance) or better in 55% of cases and within 1D (Correlates to 20/40 when targeted for distance) or better in 85% of cases. Recent developments in interoperative wavefront technology such as the ORA System from Wavetec Vision Systems, have demonstrated in studies to provide power calculations that lead to improved outcomes, yielding 80% of patients within 0.5D (20/25 or better).
Statistically, cataract surgery and IOL implantation seem to be ones of the safest and with highest success rates procedures when it comes to eye care. However as any other type of surgery it implies certain risks. The cost is another important aspect of these lenses. Although most insurance companies cover the costs of traditional IOLs, patients may need to pay the price-difference in case they choose more advanced lenses, such as the premium ones.
Preoperative evaluation
An eye examination or pre-operative evaluation by an eye surgeon is necessary to confirm the presence of a cataract and to determine if the patient is a suitable candidate for surgery. The patient must fulfill certain requirements such as:
- The degree of reduction of vision due, at least in large part, to the cataract should be evaluated. While the existence of other sight-threatening diseases, such as age-related macular degeneration or glaucoma, does not preclude cataract surgery, less improvement may be expected in their presence.
- The eyes should have a normal pressure, or any pre-existing glaucoma should be adequately controlled on medications. In cases of uncontrolled glaucoma, a combined cataract-glaucoma procedure (Phaco-trabeculectomy) can be planned and performed.
- The pupil should be adequately dilated using eyedrops; if pharmacologic pupil dilation is inadequate, procedures for     mechanical pupillary dilatation may be needed during the surgery.
- The patients with retinal detachment may be scheduled for a combined vitreo-retinal procedure, along with PC-IOL implantation.
- In addition, it has recently been shown that patients taking tamsulosin (Flomax), a common drug for enlarged prostate, are prone to developing a surgical complication known as intraoperative floppy iris syndrome (IFIS), which must be correctly managed to avoid the complication posterior capsule rupture; however, prospective studies have shown that the risk is greatly reduced if the surgeon is informed of the patient’s history with the drug beforehand, and has appropriate alternative techniques prepared.
Operation procedures
The surgical procedure in phacoemulsification for removal of cataract involves a number of steps. Each step must be carefully and skillfully performed in order to achieve the desired result. The steps may be described as follows:
- Anaesthesia,
- Exposure of the eyeball using a lid speculum,
- Entry into  the eye through a minimal incision (corneal or scleral)
- Viscoelastic injection to stabilize the anterior chamber and to help maintain the eye pressurization
- Capsulorhexis
- Hydrodissection pie
- Hydro-delineation
- Ultrasonic destruction or emulsification of the cataract after nuclear cracking or  chopping (if needed), cortical aspiration of the remanescent lens, capsular polishing (if needed)
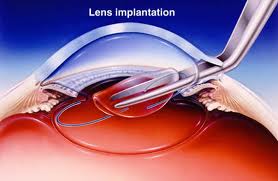
- Implantation of the, usually foldable, intra-ocular lens (IOL)
- Viscoelastic removal
- Wound sealing / hydration (if needed).
 The pupil is dilated using drops (if the IOL is to be placed behind the iris) to help better visualise the cataract. Pupil-constricting drops are reserved for secondary implantation of the IOL in front of the iris (if the cataract has already been removed without primary IOL implantation). Anesthesia may be placed topically (eyedrops) or via injection next to (peribulbar) or behind (retrobulbar) the eye. Oral or intravenous sedation may also be used to reduce anxiety. General anesthesia is rarely necessary, but may be employed for children and adults with particular medical or psychiatric issues. The operation may occur on a stretcher or a reclining examination chair. The eyelids and surrounding skin will be swabbed with disinfectant. The face is covered with a cloth or sheet, with an opening for the operative eye. The eyelid is held open with a speculum to minimize blinking during surgery. Pain is usually minimal in properly anesthetised eyes, though a pressure sensation and discomfort from the bright operating microscope light is common. The ocular surface is kept moist using sterile saline eyedrops or methylcellulose viscoelastic. The discission into the lens of the eye is performed at or near where the cornea and sclera meet (limbus = corneoscleral junction). Advantages of the smaller incision include use of few or no stitches and shortened recovery time. A capsulotomy (rarely known as cystotomy) is a procedure to open a portion of the lens capsule, using an instrument called a cystotome. An anterior capsulotomy refers to the opening of the front portion of the lens capsule, whereas a posterior capsulotomy refers to the opening of the back portion of the lens capsule. In phacoemulsification, the surgeon performs an anterior continuous curvilinear capsulorhexis, to create a round and smooth opening through which the lens nucleus can be emulsified and the intraocular lens implant inserted.
The pupil is dilated using drops (if the IOL is to be placed behind the iris) to help better visualise the cataract. Pupil-constricting drops are reserved for secondary implantation of the IOL in front of the iris (if the cataract has already been removed without primary IOL implantation). Anesthesia may be placed topically (eyedrops) or via injection next to (peribulbar) or behind (retrobulbar) the eye. Oral or intravenous sedation may also be used to reduce anxiety. General anesthesia is rarely necessary, but may be employed for children and adults with particular medical or psychiatric issues. The operation may occur on a stretcher or a reclining examination chair. The eyelids and surrounding skin will be swabbed with disinfectant. The face is covered with a cloth or sheet, with an opening for the operative eye. The eyelid is held open with a speculum to minimize blinking during surgery. Pain is usually minimal in properly anesthetised eyes, though a pressure sensation and discomfort from the bright operating microscope light is common. The ocular surface is kept moist using sterile saline eyedrops or methylcellulose viscoelastic. The discission into the lens of the eye is performed at or near where the cornea and sclera meet (limbus = corneoscleral junction). Advantages of the smaller incision include use of few or no stitches and shortened recovery time. A capsulotomy (rarely known as cystotomy) is a procedure to open a portion of the lens capsule, using an instrument called a cystotome. An anterior capsulotomy refers to the opening of the front portion of the lens capsule, whereas a posterior capsulotomy refers to the opening of the back portion of the lens capsule. In phacoemulsification, the surgeon performs an anterior continuous curvilinear capsulorhexis, to create a round and smooth opening through which the lens nucleus can be emulsified and the intraocular lens implant inserted.