Female Condoms at a Glance
- A pouch inserted into the vagina to prevent pregnancy
- Reduces the risk of sexually transmitted infection
- Can be used for vaginal and anal intercourse
- Safe, effective, and convenient
- Easy to get
- Cost about $4 each
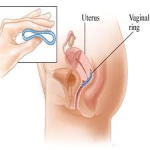
Vaginal Ring at a Glance
- A small ring you put in your vagina once a month for three weeks to prevent pregnancy
- Safe, effective, and convenient
- Easy to get with a prescription
- Costs about $15–$80 a month
·        How Does the Vaginal Ring Work?
 Like other methods of birth control, NuvaRing releases hormones. Hormones are chemicals made in our bodies. They control how different parts of our bodies work.
Like other methods of birth control, NuvaRing releases hormones. Hormones are chemicals made in our bodies. They control how different parts of our bodies work.
The hormones in NuvaRing are the same hormones as in the birth control pill — estrogen and progestin.
The hormones work by keeping a woman’s ovaries from releasing eggs — ovulation. Pregnancy cannot happen if there is no egg to join with sperm. The hormones in NuvaRing also prevent pregnancy by thickening a woman’s cervical mucus. The mucus blocks sperm and keeps it from joining with an egg.
The hormones also thin the lining of the uterus. In theory, this could prevent pregnancy by keeping a fertilized egg from attaching to the uterus.
What works and what doesn’t?
With the exception of Withdrawal (coitus interruptus), the above methods have the blessing of family planning experts because when used properly, they prevent pregnancy.
However, while the rhythm method is okay for well-motivated couples who have been trained in its use by a qualified ‘natural family planning’ teacher, for the rest of us, it’s a bit risky.
Also very risky are certain non-approved methods, for instance, using spermicides (chemical pessaries, creams or foams), or douching your vagina after sex.
Practices like ‘doing it standing up’ or ‘coughing a lot afterwards’ or ‘trying not to come’ don’t work, and will simply lead to unwanted pregnancy.
How effective are the various methods?
 Some contraceptive methods are more effective in preventing pregnancy than others, while only condoms offer any protection against sexually transmitted infections.
Some contraceptive methods are more effective in preventing pregnancy than others, while only condoms offer any protection against sexually transmitted infections.
The following figures will give you some idea of which kinds of contraception are the most efficient at protecting you against pregnancy.
Table 2: Effectiveness of contraceptive methods.
|
Contraceptive  method |
Effectiveness |
| Vasectomy | Almost 100 per cent |
| Female sterilisation | Almost 100 per cent |
| The Pill | Almost 100 per cent |
| Contraceptive injection | Almost 100 per cent |
| IUS (Mirena) | 98 to 99 per cent |
| IUD (the coil) | 97 to 98 per cent |
| The mini-Pill | Around 98 per cent |
| Male condom | 90 to 98 per cent |
| Female condom | 90 to 98 per cent |
| Diaphragm with spermicide | 90 to 96 per cent |
None of the methods is quite 100 per cent effective, which means the only guaranteed way of preventing conception is to not have sex!
You should also remember that some methods are quite complicated to use, and no method is as safe as the figures quoted if you don’t follow the instructions carefully.
For example, if you are taking the Pill, you shouldn’t miss taking a tablet. If you are using condoms, you should make sure you put them on before sex starts – not half way through. If you’re relying on the contraceptive injection, you do need to turn up for your jab on time.
Every method, except vasectomy and sterilisation, can fail if you don’t take care.
What about new methods of contraception?
Other methods of contraception will be available in the future. Below is a recent development.
The male Pill
Research work continues on the male Pill, particularly in California and in China.
Alas, it’s still at least five years away from general release, despite the fact that it keeps making optimistic headlines in the newspapers.
At present, it’s an injection, or an implant or patch, not a pill.
Among the difficulties is the fact that hormones which reduce sperm production may also reduce sexual desire.
It’s unlikely to reach the British market before 2016.
Where do I get advice about choosing a contraceptive?
 The UK has very good, free contraceptive services.
The UK has very good, free contraceptive services.
Traditionally, advice has been provided by the specially-trained experts at Britain’s large chain of family planning clinics, which were originally set up by the Family Planning Association (FPA).
About 1.1 million women (and 162,000 men) attended family planning clinics. Substantially larger numbers of people got contraceptive help from general practitioners.
You can find your local FP clinic in the phone book, or use the ‘clinic finder’ on the FPA website.
Alternatively, these days, nearly all GPs also offer advice on contraception.
If you don’t want to talk to your own doctor about family planning, you can ask to see another. You can even go to a different practice if you want to, though that’s rarely done.
It’s fair to say that many GPs aren’t experts in all methods of family planning. But often there is one partner in the practice who does have good qualifications in contraception.
If you’re under 25, you could also go to a Brook advisory clinic or a local youth advice clinic.
