The International Federation of Gynecology and Obstetrics (FIGO) staging systems for vulva, cervix, endometrium, and sarcomas have been revised for the first time in over a decade. The purpose of the staging system is to provide uniform terminology for better communication among health professionals and to provide appropriate prognosis to the patients which results in treatment improvement. This is a constantly evolving process as new therapeutic modalities are developed, new imaging and surgical approaches are applied, and more prognostic information becomes available. The previous system did not reflect the prognosis in some patient subsets where medical research and practice have shown explosive growth of new knowledge in recent years.Â
 The 41st Annual Meeting of the Society of Gynecologic Oncologists was held in March 2010. Several abstracts reported retrospective studies that evaluated the prognostic significance of new 2009 FIGO staging guidelines compared to the old 1988 FIGO system. In endometrial cancer, the reduction in the substages within stage I, and the separation of pelvic and para-aortic nodal involvement further clarified important prognostic factors that yielded clear delineation of survival.
The 41st Annual Meeting of the Society of Gynecologic Oncologists was held in March 2010. Several abstracts reported retrospective studies that evaluated the prognostic significance of new 2009 FIGO staging guidelines compared to the old 1988 FIGO system. In endometrial cancer, the reduction in the substages within stage I, and the separation of pelvic and para-aortic nodal involvement further clarified important prognostic factors that yielded clear delineation of survival.
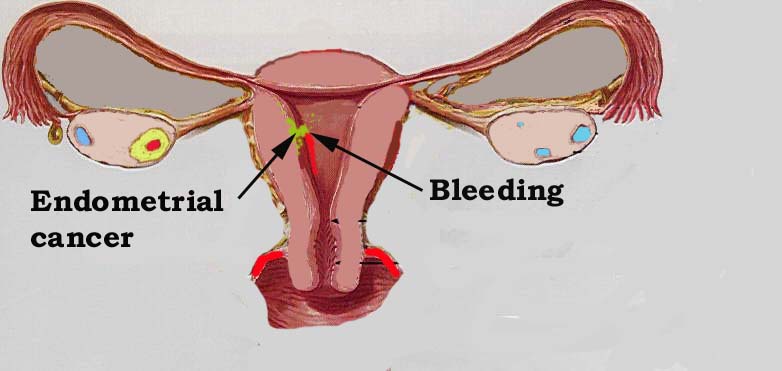
Carcinoma of the Endometrium
IA        Tumor confined to the uterus, no or < ½ myometrial invasion
IB        Tumor confined to the uterus, > ½ myometrial invasion
IIÂ Â Â Â Â Â Â Â Â Cervical stromal invasion, but not beyond uterus
IIIAÂ Â Â Â Â Tumor invades serosa or adnexa
IIIBÂ Â Â Â Â Vaginal and/or parametrial involvement
IIIC1Â Â Â Pelvic node involvement
IIIC2Â Â Â Para-aortic involvement
IVAÂ Â Â Â Â Â Tumor invasion bladder and/or bowel mucosa
IVBÂ Â Â Â Â Â Distant metastases including abdominal metastases and/or inguinal lymph nodes
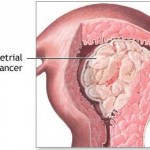 Most endometrial cancers are carcinomas (usually adenocarcinomas), meaning that they originate from the single layer of epithelial cells that line the endometrium and form the endometrial glands. There are many microscopic subtypes of endometrial carcinoma, including the common endometrioid type, in which the cancer cells grow in patterns reminiscent of normal endometrium, and the far more aggressive papillary serous carcinoma and clear cell endometrial carcinomas. Some authorities have proposed that endometrial carcinomas be classified into two pathogenetic groups.
Most endometrial cancers are carcinomas (usually adenocarcinomas), meaning that they originate from the single layer of epithelial cells that line the endometrium and form the endometrial glands. There are many microscopic subtypes of endometrial carcinoma, including the common endometrioid type, in which the cancer cells grow in patterns reminiscent of normal endometrium, and the far more aggressive papillary serous carcinoma and clear cell endometrial carcinomas. Some authorities have proposed that endometrial carcinomas be classified into two pathogenetic groups.
- Type I: These cancers occur most commonly in pre- and peri-menopausal women, often with a history of unopposed estrogen exposure and/or endometrial hyperplasia. They are often minimally invasive into the underlying uterine wall, are of the low-grade endometrioid type, and carry a good prognosis.
- Type II: These cancers occur in older, post-menopausal women, are more common in African-Americans, are not associated with increased exposure to estrogen, and carry a poorer prognosis. They include:
- the high-grade endometrioid cancer,
- the uterine papillary serous carcinoma,
- the uterine clear cell carcinoma.
Treatment options by stage
Stage I
- Surgery
- Surgery and radiation therapy
- Hormone therapy
- Surgery, radiation, and chemotherapy
Stage II
- Surgery and radiation therapy
- Surgery, radiation, and chemotherapy
Stage III
- Surgery and radiation therapy
- Surgery and chemotherapy
- Surgery, radiation, and chemotherapy
Stage IV
- Surgery
- Radiation therapy
- Hormone therapy
- Chemotherapy
 Surgery
Surgery
Surgery is the removal of the tumor and surrounding tissue during an operation. Surgery is typically the first treatment used for uterine cancer. A surgical oncologist is a doctor who specializes in treating cancer using surgery. Depending on the extent of the cancer, the surgeon will perform either a simple hysterectomy (removal of the body of the uterus and cervix) or a radical hysterectomy (removal of the uterus, cervix, the upper part of the vagina, and nearby tissues). In addition, the surgeon will remove lymph nodes near the tumor to determine if the cancer has spread beyond the uterus. The surgeon will also perform a bilateral salpingo-oophorectomy (removal of both fallopian tubes and ovaries) for patients who have been through menopause.
Radiation therapy
Radiation therapy is the use of high-energy x-rays or other particles to kill cancer cells. A doctor who specializes in giving radiation therapy to treat cancer is called a radiation oncologist. A radiation therapy regimen (schedule) usually consists of a specific number of treatments given over a set period of time. The most common type of radiation treatment is called external-beam radiation therapy, which is radiation given from a machine outside the body.
Chemotherapy
Chemotherapy is the use of drugs to kill cancer cells, usually by stopping the cancer cells’ ability to grow and divide. Systemic chemotherapy is delivered through the bloodstream to reach cancer cells throughout the body. Chemotherapy is given by a medical oncologist, a doctor who specializes in treating cancer with medication. A chemotherapy regimen (schedule) usually consists of a specific number of cycles given over a set period of time. A patient may receive one drug at a time or combinations of different drugs at the same time.
Hormone therapy
Hormone therapy is used to slow the growth of uterine cancer cells. Hormone therapy for uterine cancer involves the sex hormone progesterone, given in a pill form. Other hormone therapies are tamoxifen (Nolvadex) and aromatase inhibitors (AIs), such as anastrozole (Arimidex), letrozole (Femara), and exemestane (Aromasin). An AI is a drug that reduces the amount of the hormone estrogen in a woman’s body by stopping tissues and organs other than the ovaries from producing it. Hormone therapy may be used for women who cannot have surgery or radiation therapy, as well as in combination with other types of treatment.