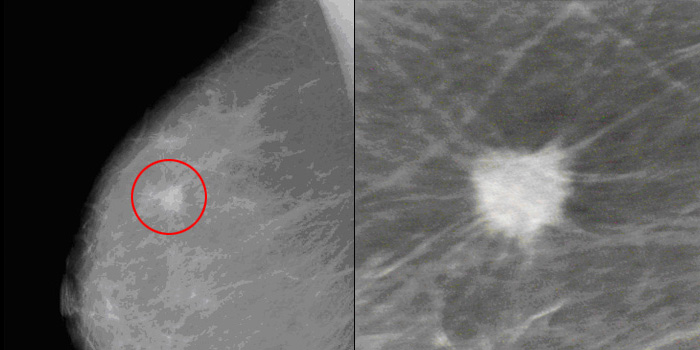
One of the scariest things a woman can hear is that her mammogram shows a suspicious mass in her breast. That news can shake a woman’s sense of well-being even after further testing fails to find breast cancer.
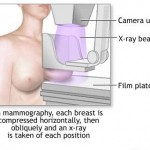
It’s important to remember that a mammogram is a screening test. A screening test is done to look for disease in someone who doesn’t have any symptoms.
At their best, screening mammograms can find breast cancer early. But an abnormal result by itself does not mean cancer. It just means that follow-up testing is needed. In many cases, the abnormal mammogram turns out to be a false alarm.
What tests are done after an abnormal mammogram?
Tests that may be done after an abnormal mammogram include:
- Ultrasound of the breast, which can show more-detailed pictures of the breast tissue.
- Diagnostic mammography. In most cases, two pictures of each breast are taken for a screening mammogram. For a diagnostic mammogram, many more pictures are made of the breast, focusing on the area of concern.
- Biopsy to remove fluid or tissue to check it for cancer cells. Tissue may be removed using surgery (excisional biopsy) or a needle (fine needle aspiration or core needle biopsy).
The biopsy performed can be needle biopsy. Needle biopsies include:
- Fine needle aspiration
- Core needle biopsy
- Mammotome (vacuum assisted large core needle) biopsy
- Needle/hookwire localisation biopsy
- Stereotactic localisation biopsy
Localisation procedures would be followed by surgery.
These can be performed as an office procedure/outpatient clinic setting. That means, you do not need to be admitted but it can be done in the mammography suite or ultrasound room. No special preparations are also necessary and you can return home almost immediately after the procedure.
Fine needle aspiration cytology (FNAC) deserves further mention. It involves aspirating cells with a fine needle from the lump or abnormal area in the breast, with a syringe, spreading the cells onto a slide and examining the cells with a microscope.  As mentioned above, this can be can be done in the outpatient clinic, is rapid and relatively painless.  However it requires an experienced cytopathologist. In a specialised clinic (usually called the Breast Clinic), an immediate report can be given, reducing the waiting time for the result, a period which can be very distressing for the woman. This is currently the biopsy method used in breast clinics around the world.  Combined with clinical examination and mammography (known as “triple assessmentâ€) the accuracy is nearly 99%.
Core needle biopsy involves sampling with a larger bore needle. A local anaesthetic is necessary and the results are not immediate. However, this gives a larger sample of tissue for diagnosis by the pathologist.
In all lesions that are not palpable, the needle biopsy or localisation biopsy will be done under ultrasound or mammography guidance, depending on whether the lesion is visible by ultrasound or mammography. If the lesion were visible on both mammography and ultrasound, ultrasound would be the choice for guiding the biopsy in most centres.
 Some patients will have a surgical biopsy done following the detected abnormality, if the lesion is palpable or after a needle localisation procedure. Surgical biopsies can either be excisional or incisional. An excisional biopsy with clear margins is similar to a lumpectomy. This involves anaesthesia and a second definitive operation is necessary, if the results are malignant (cancerous).
Some patients will have a surgical biopsy done following the detected abnormality, if the lesion is palpable or after a needle localisation procedure. Surgical biopsies can either be excisional or incisional. An excisional biopsy with clear margins is similar to a lumpectomy. This involves anaesthesia and a second definitive operation is necessary, if the results are malignant (cancerous).
Depending on whether the lesion tested, turns out to be cancer or not, the flow of events may include follow up mammograms and/or ultrasound, repeat biopsy or just routine follow up. The following flow chart only serves as a guide.
Remember that each patient is unique and will have their recommendations tailored to themselves and their condition. Do be surprised if your friend or relative may not have undergone similar tests for an abnormality of their breast.
A biopsy is the only sure way to diagnose breast cancer. About 8 out of 10 breast changes that are biopsied are found to be benign (not cancer).
What accounts for the high rate of abnormal mammograms that aren’t cancer?
If a test shows a problem when none exists, the result is called a “false-positive.” A false-positive mammogram may occur because:
- The mass that was found is something besides cancer, or
- Normal tissue appears as abnormal
Also, a woman’s age and type of breast tissue are factors in the false-positive rate. A woman is more likely to get a false-positive result if she:
- Is young (younger women tend to have denser breast tissue)
- Has a history of breast biopsies
- Has a family history of breast cancer
- Is taking hormone replacement therapy
Experts estimate that the chance of getting a false-positive from a screening mammogram is about 1 in 10. This increases over time. Among women who get a screening mammogram every year for 10 years, about half of them will be sent for further testing that turns out to be a false alarm. Often this just means that more x-ray views will be taken.
Why should I get mammograms?
It can be frightening to get a false-positive result and then go through follow-up testing. It might make a woman question the value of the whole experience.
Mammograms aren’t perfect. But keep in mind these important facts:
- Mammograms are the best tool we have to find breast cancer early. Mammography combined with clinical breast exam can find up to 95 percent of breast cancers.
- Mammograms have been proven to cut cancer deaths. They do this by finding cancer in its early stages, when treatment is most likely to be effective.
- Mammograms often find breast cancer years before a lump can be felt. Checking your own breasts for changes may be helpful, but breast self-exams should not take the place of regular mammograms and clinical breast exams.
When you should start getting mammograms depends on many factors, including your age, risk for breast cancer, and personal and family medical history. Talk to your doctor about the best screening schedule for you.