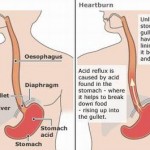
Heartburn, also known as pyrosis or acid indigestion is a burning sensation in the chest, just behind the breastbone or in the epigastrium. The pain often rises in the chest and may radiate to the neck, throat, or angle of the jaw.
 Heartburn is usually associated with regurgitation of gastric acid (gastric reflux) which is the major symptom of gastroesophageal reflux disease (GERD). It however may also be a symptom of ischemic heart disease so concluding that it is gastroesophageal reflux disease prematurely may lead to misdiagnosis.
Heartburn is usually associated with regurgitation of gastric acid (gastric reflux) which is the major symptom of gastroesophageal reflux disease (GERD). It however may also be a symptom of ischemic heart disease so concluding that it is gastroesophageal reflux disease prematurely may lead to misdiagnosis.
The terms dyspepsia and indigestion are often used interchangeably with heartburn, though some sources emphasize a distinction. Dyspepsia is defined as a combination of epigastric pain and heartburn. Heartburn is commonly used interchangeably with gastroesophageal reflux disease rather than just to describe a symptom of burning in one’s chest.
Differential diagnosis
Cardiac and esophageal causes may share similar symptoms as these two structures have the same nerve supply.
 Cardiac disease is one of the first conditions that must be excluded in patients with unexplained chest pain given that patients with chest pain related to GERD cannot be distinguished from those with chest pain due to cardiac conditions. As many as 30% of chest pain patients undergoing cardiac catheterization have findings which do not account for their chest discomfort, and are often defined as having “atypical chest pain” or chest pain of undetermined origin. According to data recorded in several studies based on ambulatory pH and pressure monitoring, it is estimated that 25% to 50% of these patients have evidence of abnormal GERD.
Cardiac disease is one of the first conditions that must be excluded in patients with unexplained chest pain given that patients with chest pain related to GERD cannot be distinguished from those with chest pain due to cardiac conditions. As many as 30% of chest pain patients undergoing cardiac catheterization have findings which do not account for their chest discomfort, and are often defined as having “atypical chest pain” or chest pain of undetermined origin. According to data recorded in several studies based on ambulatory pH and pressure monitoring, it is estimated that 25% to 50% of these patients have evidence of abnormal GERD.
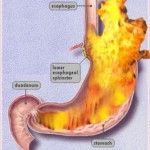
GERD
Gastroesophageal reflux disease is the most common cause of heartburn. In this condition acid reflux has led to inflammation of the esophagus.
Functional heartburn
Functional heartburn is heartburn of unknown cause. It is associated with other functional gastrointestinal disorder like irritable bowel syndrome and is the primary cause of lack of improvement post treatment with proton pump inhibitors (PPIs). PPIs are however still the primary treatment with response rates in about 50% of people. The diagnosis is based upon the Rome III criteria of
1) burning retrosternal discomfort
2) absence of GERD as the cause
3) no esophageal motility disorders.
It was found to be present in 22.3% of Canadians in one survey.
Cardiac
Heartburn is recognized as a symptom of an acute myocardial infarction and angina. A description of burning or indigestion-like pain increases the risk of acute coronary syndrome, but not to a statistically significant level. In a group of people presenting to a hospital with GERD symptoms, 0.6% may be due to ischemic heart disease.
Diagnostic approach
Heartburn can be caused by several conditions and a preliminary diagnosis of GERD is based on additional signs and symptoms. The chest pain caused by GERD has a distinct ‘burning’ sensation, occurs after eating or at night, and worsens when a person lies down or bends over. It also is common in pregnant women, and may be triggered by consuming food in large quantities, or specific foods containing certain spices, high fat content, or high acid content. If the chest pain is suspected to be heartburn, patients may undergo an upper GI series to confirm the presence of acid reflux. Heartburn or chest pain after eating or drinking and combined with difficulty swallowing may indicate esophageal spasms.
GI cocktail
Relief of symptoms 5 to 10 minutes after the administration of viscous lidocaine and an antacid increases the suspicion that the pain is esophageal in origin. This however does not rule out a potential cardiac cause as 10% of cases of discomfort due to cardiac causes are improved with antacids.
Biochemical
Esophageal pH monitoring : A probe can be placed via the nose into the esophagus to record the level of acidity in the lower esophagus. Because some degree of variation in acidity is normal, and small reflux events are relatively common, esophageal pH monitoring can be used to document reflux in real-time.
Mechanical
Manometry : In this test, a pressure sensor (manometer) is passed through the mouth into the esophagus and measures the pressure of the lower esophageal sphincter directly.
Endoscopy : The esophageal mucosa can be visualized directly by passing a thin, lighted tube with a tiny camera known as an endoscope attached through the mouth to examine the esophagus and stomach. In this way, evidence of esophageal inflammation can be detected, and biopsies taken if necessary. Since an endoscopy allows a doctor to visually inspect the upper digestive tract the procedure may help identify any additional damage to the tract that may not have been detected otherwise.
Biopsy : A small sample of tissue from the esophagus is removed. It is then studied to check for inflammation, cancer, or other problems.
Treatment
The treatment of heartburn depends on the underlying cause. Medicines such as H2 receptor antagonists or proton pump inhibitors are effective for gastritis and GERD, the two most common causes of heartburn. Antibiotics are used if H. pylori is present.
Epidemiology
About 42% of the United States population has had heartburn at some point.