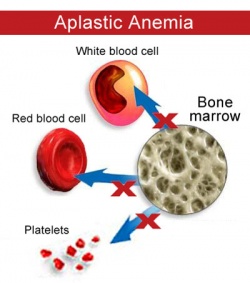
Aplastic anemia is a condition where bone marrow does not produce sufficient new cells to replenish blood cells. The condition, per its name, involves both aplasia and anemia. Typically, anemia refers to low red blood cell counts, but aplastic anemia patients have lower counts of all three blood cell types: red blood cells, white blood cells, and platelets, termed pancytopenia.
Signs and symptoms
- Anemia with malaise, pallor and associated symptoms such as palpitations
- Thrombocytopenia (low platelet counts), leading to increased risk of hemorrhage, bruising and petechiae
- Leukopenia (low white blood cell count), leading to increased risk of infection
- Reticulocytopenia (low reticulocyte counts)
Causes
In many cases, the etiology is considered to be idiopathic (without a known cause), but one known cause is an autoimmune disorder in which white blood cells attack the bone marrow.
Aplastic anemia is also sometimes associated with exposure to toxins such as benzene, or with the use of certain drugs, including chloramphenicol, carbamazepine, felbamate, phenytoin, quinine, and phenylbutazone. Many drugs are associated with aplasia mainly according to case reports but at a very low probability. As an example, chloramphenicol treatment is followed by aplasia in less than 1 in 40,000 treatment courses, and carbamazepine aplasia is even more rare.
Exposure to ionizing radiation from radioactive materials or radiation-producing devices is also associated with the development of aplastic anemia. Marie Curie, famous for her pioneering work in the field of radioactivity, died of aplastic anemia after working unprotected with radioactive materials for a long period of time; damaging effects of ionizing radiation were not then known.
Aplastic anemia is present in up to 2% of patients with acute viral hepatitis.
In some animals aplastic anemia may have other causes. For example, in the ferret (Mustela putorius furo) aplastic anemia is caused by estrogen toxicity. This is because female ferrets are induced ovulators, so mating is required to bring the female out of heat. Intact females, if not mated, will remain in heat, and after some time the high levels of estrogen will cause the bone marrow to stop producing red blood cells.
Short-lived aplastic anemia can also be a result of parvovirus infection. In humans the P antigen (also known as globoside) is the cellular receptor for parvovirus B19 virus that causes erythema infectiosum (fifth disease) in children. Parvovirus causes complete cessation of red blood cell production. In most cases, this goes unnoticed, as red blood cells live for up to 180 days, and the drop in production does not significantly affect the total number of circulating red blood cells. In people with conditions where the cells die early (such as sickle cell disease), however, parvovirus infection can lead to severe anemia.
Treatment
Treating immune-mediated aplastic anemia involves suppression of the immune system, an effect achieved by daily medicine intake, or, in more severe cases, a bone marrow transplant, a potential cure. The transplanted bone marrow replaces the failing bone marrow cells with new ones from a matching donor. The multipotent stem cells in the bone marrow reconstitute all three blood cell lines, giving the patient a new immune system, red blood cells, and platelets. However, besides the risk of graft failure, there is also a risk that the newly created white blood cells may attack the rest of the body (“graft-versus-host disease”).
Medical therapy of aplastic anemia often includes a short course of anti-thymocyte globulin (ATG) or anti-lymphocyte globulin (ALG) and several months of treatment with cyclosporin to modulate the immune system. Mild chemotherapy with agents such as cyclophosphamide and vincristine may also be effective. Antibody therapy, such as ATG, targets T-cells, which are believed to attack the bone marrow. Steroids are generally ineffective, though are often used to combat serum sickness caused by ATG use.
One prospective study involving cyclophosphamide was terminated early due to a high incidence of mortality, due to severe infections as a result of prolonged neutropenia.
In the past, before the above treatments became available, patients with low leukocyte counts were often confined to a sterile room or bubble (to reduce risk of infections), as in the famed case of Ted DeVita.
Follow-up
Regular full blood counts are required to determine whether the patient is still in a state of remission.
10-33% of all patients develop the rare disease paroxysmal nocturnal hemoglobinuria (PNH, anemia with thrombopenia and/or thrombosis), which has been explained as an escape mechanism by the bone marrow against destruction by the immune system. Flow cytometry testing is performed regularly in people with previous aplastic anemia to monitor for the development of PNH.