Bedsores, more properly known as pressure ulcers or decubitus ulcers, are lesions caused by many factors—such as unrelieved pressure, friction, humidity, shearing forces, temperature, age, continence, and medication—to any part of the body, especially portions over bony or cartilaginous areas such as sacrum, elbows, knees, and ankles. Although often prevented and treatable if found early, they can be very difficult to prevent in frail elderly patients, wheelchair users (especially where spinal injury is involved) and terminally ill patients.
 Bedsores are often fatal—even under the auspices of medical care—and are one of the leading iatrogenic causes of death reported in developed countries, second only to adverse drug reactions. The primary cure and treatment is to remove the pressure by turning the patient regularly (every two hours is often quoted, though the evidence for this figure is not strong and four hourly turns may be as effective in some patients). However the relief of pressure to avoid further sores is well documented since at least the 19th century; regular turning was advised to prevent sores by Galloway (though some of her other recommendations are not current practice, for example massage of the pressure area is probably contra-indicated) and virtually all authors since.
Bedsores are often fatal—even under the auspices of medical care—and are one of the leading iatrogenic causes of death reported in developed countries, second only to adverse drug reactions. The primary cure and treatment is to remove the pressure by turning the patient regularly (every two hours is often quoted, though the evidence for this figure is not strong and four hourly turns may be as effective in some patients). However the relief of pressure to avoid further sores is well documented since at least the 19th century; regular turning was advised to prevent sores by Galloway (though some of her other recommendations are not current practice, for example massage of the pressure area is probably contra-indicated) and virtually all authors since.
Classification
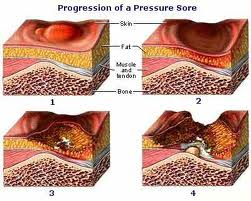
The definitions of the four pressure ulcer stages are revised periodically by the National Pressure Ulcer Advisory Panel (NPUAP) in the United States. Briefly, however, they are as follows:
- Stage I is the most superficial, indicated by non blanchable redness that does not  subside after pressure is relieved. This stage is visually similar to reactive hyperemia seen in skin after prolonged application of pressure. Stage I pressure ulcers can be  distinguished from reactive hyperemia in two ways:
- a) reactive hyperemia resolves itself within 3/4 of the time pressure was applied, and
- b) reactive hyperemia blanches when pressure is applied, whereas a Stage I pressure ulcer does not.
- The skin may be hotter or cooler than normal, have an odd texture, or perhaps be painful to the patient. Although easy to identify on a light-skinned patient, ulcers on darker-skinned individuals may show up as shades of purple or blue in comparison to lighter skin tones.
- Stage II is damage to the epidermis extending into, but no deeper than, the dermis. In this stage, the ulcer may be referred to as a blister or abrasion.
- Stage III involves the full thickness of the skin and may extend into the subcutaneous tissue layer. This layer has a relatively poor blood supply and can be difficult to heal. At this stage, there may be undermining damage that makes the wound much larger than it may seem on the surface
- Stage IV is the deepest, extending into the muscle, tendon or even bone.
- Unstageable pressure ulcers are covered with dead cells, or eschar and wound exudate,such that the depth cannot be determined.
 Suspected Deep Tissue Injury: Purple or maroon localized area of discolored intact skin or blood-filled blister due to damage of underlying soft tissue from pressure and/or shear. The area may be preceded by tissue that is painful, firm, mushy, boggy, warmer or cooler as compared to adjacent tissue.
Suspected Deep Tissue Injury: Purple or maroon localized area of discolored intact skin or blood-filled blister due to damage of underlying soft tissue from pressure and/or shear. The area may be preceded by tissue that is painful, firm, mushy, boggy, warmer or cooler as compared to adjacent tissue.
Further description: Deep tissue injury may be difficult to detect in individuals with dark skin tones. Evolution may include a thin blister over a dark wound bed. The wound may further evolve and become covered by thin eschar. Evolution may be rapid exposing additional layers of tissue even with optimal treatment.
With higher stages, healing time is prolonged. While about 75% of Stage II ulcers heal within eight weeks, only 62% of Stage IV pressure ulcers ever heal, and only 52% heal within one year. It is important to note that pressure ulcers do not regress in stage as they heal. A pressure ulcer that is becoming shallower with healing is described in terms of its original deepest depth (e.g., healing Stage II pressure ulcer).
Etiology
 Bedsores are accepted to be caused by three different tissue forces:
Bedsores are accepted to be caused by three different tissue forces:
- Pressure, or the compression of tissues. In most cases, this compression is caused by the force of bone against a surface, as when a patient remains in a single decubitus position for a lengthy period. After an extended amount of time with decreased tissue perfusion, ischemia occurs and can lead to tissue necrosis if left untreated.
- Shear force, or a force created when the skin of a patient stays in one place as the deep fascia and skeletal muscle slide down with gravity. This can also cause the pinching off of blood vessels which may lead to ischemia and tissue necrosis.
- Friction, or a force resisting the shearing of skin. This may cause excess shedding through layers of epidermis.
