The occurrence of synchronous bilateral invasive breast cancer (SBBC) is an uncommon event. The reported incidence ranges between 0.3% and 12%. This wide range is in part due to the many definitions used to describe the entity of bilateral breast cancer. Some physicians consider a contralateral cancer diagnosed within 1 year as a synchronous bilateral breast cancer. Others narrow the definition of synchronous bilateral breast cancers to those cancers which are diagnosed within 3 months of each other.
 The following discussion will address the etiology, diagnosis, surgical management, cosmetic outcome and prognosis of patients with synchronous bilateral breast cancer.Â
The following discussion will address the etiology, diagnosis, surgical management, cosmetic outcome and prognosis of patients with synchronous bilateral breast cancer.Â
Etiology
It is likely that synchronous bilateral tumors are independent tumors rather than secondary to metastatic spread from one of the primary lesions. Characteristics, which imply independent tumors are the presence of an intra-ductal component, different histologies or different degrees of differentiation between the tumors. In a study of the chromosomal abnormalities in patients with bilateral breast cancers, the majority of contralateral tumors arose independently of the primary tumor. Only a minority of the tumors were the result of metastatic spread from the primary tumor. A metastatic mode of spread is supported by the finding of the same clonal abnormalities between the two tumors. An alternate explanation for these similar clonal abnormalities is a single-cell origin or exogenous/endogenous influences affecting both breasts simultaneously.
In bilateral breast cancer, it is important to know whether contralateral breast lesion is metastatic or second primary, but the distinction is not always easy. Chaudary et al. proposed criteria for the diagnosis of second primary breast cancer in 1984 as follows:
(i)Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â there must be in situ change in the contralateral tumor,
(ii)Â Â Â Â Â Â Â Â Â Â Â Â Â Â Â the tumor in the second breast is histologically different from the cancer in the first breast,
(iii)Â Â Â Â Â Â Â Â Â Â Â Â Â Â the degree of histological differentiation of the tumor in the second breast is distinctly greater than that of the lesion in the first breast,
(iv)Â Â Â Â Â Â Â Â Â Â Â Â Â there is no evidence of local, regional, or distant metastases from the cancer in the ipsilateral breast.
Despite novel methods such as cDNA microarray-based CGH, Chaudary’s criteria have been hitherto the most widely accepted method to distinguish second primary lesion from metastatic lesion. Using these criteria, we attempted to characterize synchronous and metachronous bilateral breast cancers.
Diagnosis
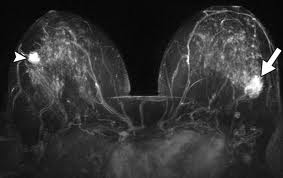
 Patients with breast cancer have an increased risk of developing either a synchronous or metachronous breast cancer which ranges between 0.5% and 0.8% each year. When patients are diagnosed with SBBC, the tumor which is diagnosed first is usually the larger tumor as compared to the contralateral tumor. The stage of the patient with SBBC is the stage of the higher staged tumor. The initial tumor is usually diagnosed by palpation, whereas, the contralateral tumor is often diagnosed by imaging modalities such as mammography, ultrasonography or magnetic resonance imaging (MRI), however, the most common mode of detection of the contralateral tumor is with mammography. This supports the role of careful screening of the contralateral breast and follow-up of all patients diagnosed with breast cancer. The most common histologic subtype is infiltrating ductal carcinoma; however, the incidence of invasive lobular carcinoma and the finding of lobular carcinoma in situ (LCIS) is slightly higher amongst synchronous bilateral carcinomas as compared to unilateral disease.
Patients with breast cancer have an increased risk of developing either a synchronous or metachronous breast cancer which ranges between 0.5% and 0.8% each year. When patients are diagnosed with SBBC, the tumor which is diagnosed first is usually the larger tumor as compared to the contralateral tumor. The stage of the patient with SBBC is the stage of the higher staged tumor. The initial tumor is usually diagnosed by palpation, whereas, the contralateral tumor is often diagnosed by imaging modalities such as mammography, ultrasonography or magnetic resonance imaging (MRI), however, the most common mode of detection of the contralateral tumor is with mammography. This supports the role of careful screening of the contralateral breast and follow-up of all patients diagnosed with breast cancer. The most common histologic subtype is infiltrating ductal carcinoma; however, the incidence of invasive lobular carcinoma and the finding of lobular carcinoma in situ (LCIS) is slightly higher amongst synchronous bilateral carcinomas as compared to unilateral disease.
Histopathologically, several studies have shown that synchronous bilateral breast tumors tend to be of lower histologic grade with a higher rate of estrogen receptor (ER) and progesterone receptor (PgR) positivity.Â
Surgical management and cosmesis
Considerable controversy has existed regarding the surgical management of patients with synchronous bilateral breast cancer. Traditionally, most clinicians have approached bilateral breast cancer more aggressively than unilateral disease. Most studies have shown a disproportionately higher incidence of bilateral mastectomy for bilateral breast cancer. This aggressive approach was employed to treat what was once thought to be a disease with a worse prognosis and outcome. However, several studies have shown that the prognosis of patients with bilateral breast cancer seems similar to unilateral disease. Gollamudi et al. retrospectively reviewed patients with SBBC and showed that they do not have a worse prognosis and can be safely treated with bilateral breast conservation. The cosmetic outcome was comparable to patients who underwent unilateral breast conservation. Heron et al. also demonstrated that bilateral breast conservation treatment does not compromise cosmesis, outcome or overall survival in this group of patients. Currently, the overall consensus is that bilateral breast cancer is amenable to bilateral breast conservation treatment without compromising survival and maintaining patient cosmesis.Â
Survival
Survival data has been difficult to interpret because of different definitions used to describe bilateral breast cancers. For example, calculations of survival from the time of the first and not the second primary can have a significant impact on the reported survival rates. There is also a question of multifocality/ multicentricity associated with these tumors affecting local recurrence rates. In a prospective study of SBBC, 18% of the bilateral breast cancer patients had the presence of multifocality on both sides. This incidence of multifocality compares with the reported incidence in many bilateral breast cancer.