A coronary stent is a tube placed in the coronary arteries that supply the heart, to keep the arteries open in the treatment of coronary heart disease. It is used in a procedure called percutaneous coronary intervention (PCI). Stents reduce chest pain and have been shown to improve survivability in the event of an acute myocardial infarction.
 Similar stents and procedures are used in non-coronary vessels e.g. in the legs in peripheral artery disease.
Similar stents and procedures are used in non-coronary vessels e.g. in the legs in peripheral artery disease.
History
The first type, developed by John Robert Dugan of Shelbyville, IN, were bare-metal stents. More recent are drug-eluting stents.
In development are stents with biocompatible surface coatings which do not elute drugs, and also absorbable stents (metal or polymer).
Placement
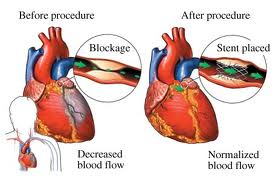 Treating a blocked (“stenosed”) coronary artery with a stent follows the same steps as other angioplasty procedures with a few important differences. The interventional cardiologist uses angiography to assess the location and estimate the size of the blockage (“lesion”) by injecting a contrast medium through the guide catheter and viewing the flow of blood through the downstream coronary arteries. Intravascular ultrasound (IVUS) may be used to assess the lesion’s thickness and hardness (“calcification”). The cardiologist uses this information to decide whether to treat the lesion with a stent, and if so, what kind and size. Drug eluting stents are most often sold as a unit, with the stent in its collapsed form attached onto the outside of a balloon catheter. Outside the US, physicians may perform “direct stenting” where the stent is threaded through the lesion and expanded. Common practice in the US is to predilate the blockage before delivering the stent. Predilation is accomplished by threading the lesion with an ordinary balloon catheter and expanding it to the vessel’s original diameter. The physician withdraws this catheter and threads the stent on its balloon catheter through the lesion. The physician expands the balloon which deforms the metal stent to its expanded size. The cardiologist may “customize” the fit of the stent to match the blood vessel’s shape, using IVUS to guide the work. It is critically important that the framework of the stent be in direct contact with the walls of the vessel to minimize potential complications such as blood clot formation. Very long lesions may require more than one stent—this result of this treatment is sometimes referred to as a “full metal jacket”.
Treating a blocked (“stenosed”) coronary artery with a stent follows the same steps as other angioplasty procedures with a few important differences. The interventional cardiologist uses angiography to assess the location and estimate the size of the blockage (“lesion”) by injecting a contrast medium through the guide catheter and viewing the flow of blood through the downstream coronary arteries. Intravascular ultrasound (IVUS) may be used to assess the lesion’s thickness and hardness (“calcification”). The cardiologist uses this information to decide whether to treat the lesion with a stent, and if so, what kind and size. Drug eluting stents are most often sold as a unit, with the stent in its collapsed form attached onto the outside of a balloon catheter. Outside the US, physicians may perform “direct stenting” where the stent is threaded through the lesion and expanded. Common practice in the US is to predilate the blockage before delivering the stent. Predilation is accomplished by threading the lesion with an ordinary balloon catheter and expanding it to the vessel’s original diameter. The physician withdraws this catheter and threads the stent on its balloon catheter through the lesion. The physician expands the balloon which deforms the metal stent to its expanded size. The cardiologist may “customize” the fit of the stent to match the blood vessel’s shape, using IVUS to guide the work. It is critically important that the framework of the stent be in direct contact with the walls of the vessel to minimize potential complications such as blood clot formation. Very long lesions may require more than one stent—this result of this treatment is sometimes referred to as a “full metal jacket”.
The procedure itself is performed in a catheterization clinic (“cath lab”). Barring complications, patients undergoing catheterizations are kept at least overnight for observation.
Dealing with lesions near branches in the coronary arteries presents additional challenges and requires additional techniques.
How long does the procedure take? It can take anywhere from 30 minutes to an hour to perform the entire case. The duration is dependent upon the technical difficulty of the case and the number of balloon catheters that have to be employed.
How safe is the procedure? In the hands of experienced cardiologists, and with availability of modern day technology, it is estimated that the risk of death is during a stent procedure is usually less than 1%, while the chance of requiring emergency bypass surgery is around 2% or less. It is a relatively safe procedure and is carried out all over the world. An “out patient” or an inpatient uncomplicated stent case usually require 23 hours or less of hospitalization after the procedure.
The risk of a other serious complication is estimated to be less than 4 and probably around 1 to 2 per thousand, and similar to that described for cardiac cath. The risk of a heart attack and bleeding that requires a blood transfusion is increased when compared to cardiac cath. However, the risks are relatively low and acceptable in most cases when one balances the potential benefit against the expected risk (risk-benefit ratio).
The aggravation of kidney function (particularly in diabetics and those with prior kidney disease) is higher than that expected with cardiac cath because of the larger amount of contrast material that is usually required. In such cases, the cardiologist takes extra precautions to prevent this possible complication.
The stent is completely covered by natural tissue in a matter of 4 – 6 weeks.and the risk of clot formation is nearly absent by that time. In very few cases (1 chance out of 200) a clot may form during the first two weeks after a stent procedure). Such patients develop symptoms of a heart attack. With prompt treatment, the majority of these stents can be reopened.
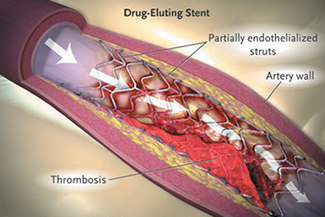
Re-occlusion
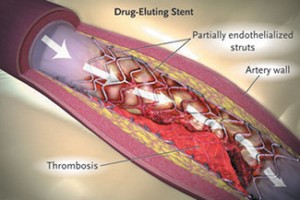 Coronary artery stents, typically a metal framework, can be placed inside the artery to help keep it open. However, as the stent is a foreign object (not native to the body), it incites an immune response. This may cause scar tissue (cell proliferation) to rapidly grow over the stent. In addition, there is a strong tendency for clots to form at the site where the stent damages the arterial wall. Since platelets are involved in the clotting process, patients must take dual antiplatelet therapy afterwards, usually clopidogrel and aspirin for one year and aspirin indefinitely. In order to reduce the treatment, new generation of stent has been developed with biodegradable polymer.
Coronary artery stents, typically a metal framework, can be placed inside the artery to help keep it open. However, as the stent is a foreign object (not native to the body), it incites an immune response. This may cause scar tissue (cell proliferation) to rapidly grow over the stent. In addition, there is a strong tendency for clots to form at the site where the stent damages the arterial wall. Since platelets are involved in the clotting process, patients must take dual antiplatelet therapy afterwards, usually clopidogrel and aspirin for one year and aspirin indefinitely. In order to reduce the treatment, new generation of stent has been developed with biodegradable polymer.
However, the dual antiplatelet therapy may be insufficient to fully prevent clots that may result in stent thrombosis; these and the cell proliferation may cause the standard (“bare-metalâ€) stents to become blocked (restenosis). Drug-eluting stents were designed to lessen this problem; by releasing an antiproliferative drug (drugs typically used against cancer or as immunosuppressants), they can help avoid this in-stent restenosis (re-narrowing).