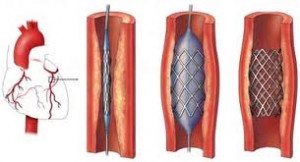
If coronary artery stenting is superior to angioplasty, why is it not used in every single case? Good question! If stents could be delivered to every lesion, and if it had the same good short and long term results in every case, it would be used in 100% cases of angioplasty. However, this is not the case. Stents are difficult to deliver across tight bends in blood vessels (particularly if they have a lot of calcium deposits in the wall) and are not usable in very small blood vessels. There are other types of technical considerations that also come into play. Today, it is estimated that stents are employed in nearly 50-75% of cases.
Controversy
 The value of stenting in rescuing someone having a heart attack (by immediately alleviating an obstruction) is clearly defined in multiple studies, but studies have failed to find reduction in hard endpoints for stents vs. medical therapy in stable angina patients (see below). The artery-opening stent can temporarily alleviate chest pain, but do not contribute to longevity. The “vast majority of heart attacks do not originate with obstructions that narrow arteries.”
The value of stenting in rescuing someone having a heart attack (by immediately alleviating an obstruction) is clearly defined in multiple studies, but studies have failed to find reduction in hard endpoints for stents vs. medical therapy in stable angina patients (see below). The artery-opening stent can temporarily alleviate chest pain, but do not contribute to longevity. The “vast majority of heart attacks do not originate with obstructions that narrow arteries.”
A more permanent and successful way to prevent heart attacks in patients at high risk is to give up smoking, exercise, and take “drugs to get blood pressure under control, drive cholesterol levels down and prevent blood clotting”.
Some cardiologists believe that stents are over-used; however, in certain patient groups, such as the elderly, GRACE and other studies have found evidence of underuse. Guidelines recommend a stress test before implanting stents, but most patients do not receive a stress test.
Clinical Trials
 While revascularisation (by stenting or bypass surgery) is of clear benefit in reducing mortality and morbidity in patients with acute symptoms (acute coronary syndromes) including myocardial infarction, their benefit is less marked in stable patients. Clinical trials have failed to demonstrate that coronary stents improve survival over best medical treatment.
While revascularisation (by stenting or bypass surgery) is of clear benefit in reducing mortality and morbidity in patients with acute symptoms (acute coronary syndromes) including myocardial infarction, their benefit is less marked in stable patients. Clinical trials have failed to demonstrate that coronary stents improve survival over best medical treatment.
- The COURAGE trial compared PCI with optimum medical therapy. Of note, the trial excluded a large number of patients at the outset and undertook angiography in all patients at baseline, thus the results only apply to a subset of patients and should not be over-generalised. COURAGE concluded that in patients with stable coronary artery disease PCI did not reduce the death, myocardial infarction or other major cardiac events when added to optimum medical therapy.
- The MASS-II trial compared PCI, CABG and optimum medical therapy for the treatment of  multi-vessel coronary artery disease. The MASS-II trial showed no difference in cardiac death or acute MI among patients in the CABG, PCI, or MT group. However, it did show a significantly greater need for additional revascularization procedures in patients who underwent PCI.
- The SYNTAX Trialis a manufacturer-funded trial with a primary endpoint of death, cardiovascular events, and myocardial infarction, and also the need for repeat vascularization, in patients with blocked or narrowed arteries. Patients were randomized to either CABG surgery or a drug-eluding stent (the Boston Scientific TAXUS paclitaxel-eluding stent). SYNTAX found the two stratgies to be similar for hard endpoints (death and MI). Those receiving PCI required more repeat revascularisation (hence the primary endpoint analysis did not find PCI to be non-inferior), but those undergoing CABG had significantly more strokes pre or perioperatively. Use of the SYNTAX risk score is being investigated as a method of identifying those multivessel disease patients in whom PCI is a reasonable option vs those in whom CABG remains the preferred strategy.
Several other clinical trials have been performed to examine the efficacy of coronary stenting and compare with other treatment options. A consensus of the medical community does not exist.
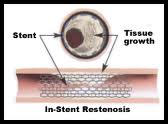
Restenosis
 One of the drawbacks of vascular stents is the potential for restenosis via the development of a thick smooth muscle tissue inside the lumen, the so-called neointima. Development of a neointima is variable but can at times be so severe as to re-occlude the vessel lumen (restenosis), especially in the case of smaller diameter vessels, which often results in reintervention. Consequently, current research focuses on the reduction of neointima after stent placement. Considerable improvements have been made, including the use of more bio-compatible materials, anti-inflammatory drug-eluting stents, resorbable stents, and others. Restenosis can be treated with a reintervention using the same method.
One of the drawbacks of vascular stents is the potential for restenosis via the development of a thick smooth muscle tissue inside the lumen, the so-called neointima. Development of a neointima is variable but can at times be so severe as to re-occlude the vessel lumen (restenosis), especially in the case of smaller diameter vessels, which often results in reintervention. Consequently, current research focuses on the reduction of neointima after stent placement. Considerable improvements have been made, including the use of more bio-compatible materials, anti-inflammatory drug-eluting stents, resorbable stents, and others. Restenosis can be treated with a reintervention using the same method.
- On September 4, 2007, an international study showed that some heart attack patients would be better off without using drug-coated stents in emergency to open their clogged arteries (patients were 5 times more likely to die after 2 years than those who received bare-metal stents). Dr. Valentin Fuster, director of the Cardiovascular Institute at Mount Sinai School of Medicine in New York said stents are less commonly used in Europe, implanted in only about 15 % of patients there while drug-lined stents are used in up to 30% of Americans having heart attacks. The new research was presented by Dr. Gabriel Steg, of the Hospital Bichat-Claude Bernard in Paris, at a meeting of the European Society of Cardiology in Vienna. Dr. Eckhart Fleck, director of cardiology at the German Heart Institute in Berlin and a spokesman for the European Society of Cardiology said that “Drug-eluting stents are not for everyone.”