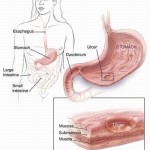
The digestive system is an intricate system that can be disrupted by disease, diet, and emotional stress. Common digestive problems such as heartburn/GERD, IBD, and IBS cause millions of Americans to suffer daily and limit quality of life. Digestive problems often result in symptoms such as bloating, diarrhea, gas, stomach pain, and stomach cramps. Learning more about the digestive system may help with managing these problems.
Reflux
 Symptoms of reflux, such as heartburn, are among the most common digestive ills. In a recent Swedish study, 6 percent of people reported experiencing reflux symptoms daily and 14 percent had them at least weekly. Such frequent symptoms may indicate a person has GERD, or gastroesophageal reflux disease. Aside from being painful, GERD can harm the esophagus over time or even lead to esophageal cancer.
Symptoms of reflux, such as heartburn, are among the most common digestive ills. In a recent Swedish study, 6 percent of people reported experiencing reflux symptoms daily and 14 percent had them at least weekly. Such frequent symptoms may indicate a person has GERD, or gastroesophageal reflux disease. Aside from being painful, GERD can harm the esophagus over time or even lead to esophageal cancer.
Heartburn typically involves a “hot or burning feeling rising up from the center of the abdomen area and into the chest under the breastbone or sternum,” says Michael Gold, director of gastroenterology at Washington Hospital Center in Washington, D.C. “It may be accompanied by a sour taste in the mouth, or hypersalivation, or even finding food or fluid in your mouth,” particularly at night. Pregnancy, some medications, and consuming alcohol or certain foods can cause heartburn. Kids under age 12 and some adults may have GERD without heartburn, instead experiencing asthmalike symptoms, trouble swallowing, or a dry cough.
Treatment options include drugs that reduce acid levels, such as the proton pump inhibitors Aciphex, Nexium, Prevacid, Prilosec, and Protonix and the H2 blockers Axid, Pepcid, Tagamet, and Zantac. But taking medication is not without risk. This November, a study found that a proton pump inhibitor may weaken the heart-protective effect of the blood thinner Plavix in patients taking both medications.
In severe cases of GERD, surgeons can tighten a loose muscle between the stomach and esophagus to inhibit the upward flow of acid. Recently, laparoscopic surgery, which involves small incisions, was found to lessen scarring and shorten recovery time compared with open procedures.
Peptic Ulcers
 If you have unexplained stomach pain, consider this before reaching for a painkiller: “The worst thing to do if ulcers are suspected is to take aspirin or other NSAID [nonsteroidal anti-inflammatory drug] pain reducers,” Gold says. “They worsen it and don’t help.”
If you have unexplained stomach pain, consider this before reaching for a painkiller: “The worst thing to do if ulcers are suspected is to take aspirin or other NSAID [nonsteroidal anti-inflammatory drug] pain reducers,” Gold says. “They worsen it and don’t help.”
Instead, if you think you have a peptic ulcer—and 25 million living Americans will get one at some point—consider getting tested for Helicobacter pylori, experts advise. By disrupting a protective layer of mucus, that bacterium causes ulcers, which are sores in the lining of the stomach or first stretch of the small intestine. Other causes include smoking, which can elevate stomach acidity, and excessive NSAID use. Alcohol use may also be a factor, but it’s unclear whether that alone can cause ulcers. (The old theory blaming factors like stress isn’t totally wrong: Stress can aggravate symptoms of peptic ulcers and delay healing.)
Left untreated, ulcers can cause internal bleeding and may eat a hole in the small intestine or stomach wall, which can lead to serious infection. Ulcer scar tissue can also block the digestive tract. And long-term H. pylori infection has been linked to an increased risk of gastric cancer.
Ten to 14 days of antibiotic treatment, often combined with acid reduction therapy, can rid someone of H. pylori. Surgery is an option for more severe cases. A study published in November in the World Journal of Surgery concluded that laparoscopic repair should be considered for all patients with so-called perforated ulcers.
Gallstones
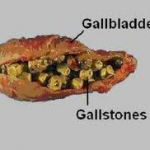 Only a quarter of people with gallstones typically require treatment. That’s fortunate, because every year nearly 1 million Americans are diagnosed with these little pebbles, which are primarily made of cholesterol and bile salts. Getting rid of them typically requires removal of the gallbladder, one of the most common U.S. surgeries.
Only a quarter of people with gallstones typically require treatment. That’s fortunate, because every year nearly 1 million Americans are diagnosed with these little pebbles, which are primarily made of cholesterol and bile salts. Getting rid of them typically requires removal of the gallbladder, one of the most common U.S. surgeries.
Gallstones can get blamed for symptoms caused by other, more elusive culprits, such as irritable bowel syndrome, says Robert Sandler, president of the American Gastroenterological Association. An ultrasound test might pick them up while missing the real problem. If you’re told you need to have gallstones out but they’re not bothering you, get a second opinion, he advises.
Removal may be necessary if the stones instigate inflammation or infection of the gallbladder, pancreas, or liver. This can happen if a stone moving out of the gallbladder gets stuck—blocking the flow of bile—in the ducts between the liver and the small intestine.
The pain of a gallstone lodged in a duct usually comes on quickly—in the right upper abdomen, between the shoulder blades, or under the right shoulder—and means a trip to the ER is needed, as may fever, vomiting, nausea, or pain lasting more than five hours. Gallbladder removal can be performed laparoscopically and more recently has been done without an external incision by going through the mouth or vagina.
Obesity is a risk factor for gallstones, and it’s theorized that they develop because of a shortage of fiber and an excess of fat in the western diet. Losing weight—then regaining it—also seems to set the stage for gallstones. In a 2006 study of men, the more frequent the weight cycling and the larger the number of pounds shed and regained, the greater the odds of gallstones. Women, especially those who are pregnant or taking birth control pills, face increases in gallstone likelihood as well.
