Between the bones of the spine (vertebrae) there is soft tissue which acts like a shock absorber. Through injury or other causes, some patients have had this material compressed, distorting the shape of the disc and causing the material to create pressure on surrounding nerves (neural impingement). Several conditions may cause such neural impingement, including spinal stenosis, disc herniation, or, rarely, tumors.
 Disc decompression is a highly effective procedure shown to be successful for 90% of patients. In this procedure, a small portion of the bone over the nerve root and/or disc material from under the nerve root is removed. This gives the nerve root more space and provide a better healing environment.
Disc decompression is a highly effective procedure shown to be successful for 90% of patients. In this procedure, a small portion of the bone over the nerve root and/or disc material from under the nerve root is removed. This gives the nerve root more space and provide a better healing environment.
There are two common types of decompression procedures:
- Microdiscectomy (or micro-decompression)
- Laminectomy (or open decompression)
Multiple clinical studies have shown that disc decompression has a high success rate, and low complication rate. This minimally invasive procedure reduces pressure on the nerve root by removing disc nucleus while preserving disc strength and future treatment options, including surgery.
Disc decompression is typically performed on an outpatient basis and requires only local anesthetic and mild sedation, alleviating the possible complications of open surgery and general anesthesia. This invasive procedure completes the continuum of care for patients who want a minimally invasive alternative to surgery.
Benefits of disc decompression include:
- Significant pain relief
- Reduced used of pain medication
- Return to previous levels of activity
- Quantifiable disc material removal
- Less scarring
- Quick recovery: generally 3-5 days
- Low complication and morbidity rates
- Outpatient procedure requiring only local anesthetic alleviates possible complications of open surgery and general anesthesia
Results compared to surgery:
- Decreased complication rate: 0.5% vs. 3% with open surgical discectomy.
- Lower re-herniation rate: 5% vs. 10-15% compared to open lumbar discectomy 21.
The microdiscectomy procedure
 A small portion of the bone over the nerve and/or disc material from under the nerve root is removed to relieve neural impingement and provide room for the nerve to heal. A microdiscectomy is typically performed for lumbar herniated disc.
A small portion of the bone over the nerve and/or disc material from under the nerve root is removed to relieve neural impingement and provide room for the nerve to heal. A microdiscectomy is typically performed for lumbar herniated disc.
A microdiscectomy surgery is more effective for treating leg pain than for lower back pain. The impingement on the nerve root can cause substantial leg pain, and while it may take weeks or months for the nerve root to fully heal and numbness or weakness get better, patients normally feel relief from leg pain almost immediately after a microdiscectomy surgery. Microdiscectomy surgery is typically recommended for patients who have experienced leg pain for at least six weeks and have not found sufficient pain relief with conservative treatment such as oral steroids, NSAID’s, and physical therapy.
Importantly, since almost all of the joints, ligaments and muscles are left intact, a microdiscectomy does not change the mechanical structure of the patient’s lower spine (lumbar spine).
Usually, a microdiscectomy procedure is performed on an outpatient basis or with one overnight stay in the hospital. Post-operatively, patients may return to a normal level of daily activity quickly.
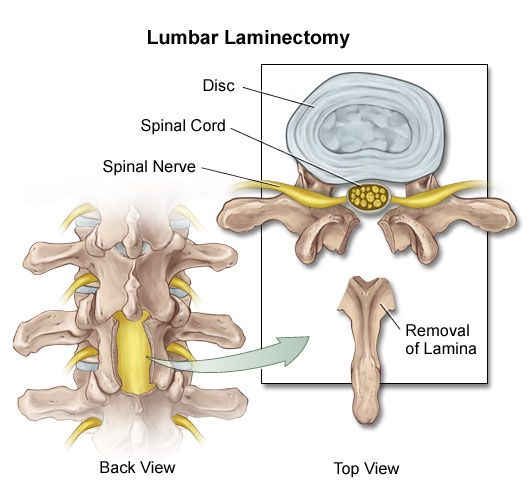
The laminectomy procedure
 A lumbar laminectomy is a surgical procedure that is performed to alleviate pain caused by neural impingement. The laminectomy surgery is designed to remove a small portion of the bone over the nerve root and/or disc material from under the nerve root to give the nerve root more space and a better healing environment.
A lumbar laminectomy is a surgical procedure that is performed to alleviate pain caused by neural impingement. The laminectomy surgery is designed to remove a small portion of the bone over the nerve root and/or disc material from under the nerve root to give the nerve root more space and a better healing environment.
A laminectomy is effective in decreasing pain and improve functions for patients with lumbar spinal stenosis, a condition that primarily afflicts elderly patients and is caused by degenerative changes that result in enlargement of the facet joints. The enlarged joints then place pressure on the nerves.
The surgical results for a laminectomy are much better for relief of leg pain caused by spinal stenosis, and not nearly as reliable for relief of lower back pain. Although removing the lamina and part of the facet joint can create more room for the nerve roots it does not eliminate the arthritis. Unfortunately, symptoms may recur after several years as the degenerative process that originally produced the spinal stenosis continues.
LASE
 LASE stands for “Laser Discectomy”, a procedure where laser light is used to correct problems with discs in the spine. The procedure is common and less invasive than other alternatives.
LASE stands for “Laser Discectomy”, a procedure where laser light is used to correct problems with discs in the spine. The procedure is common and less invasive than other alternatives.
After sedation, a miniature endoscope with a laser fiber is carefully inserted into the disc while remaining outside the spinal canal. A laser is used to remove disc tissue near the herniated site in order to decompress the disc. The procedure takes approximately one hour. Success rates are seen in about 66 – 75% of all patients who have this procedure.
The incision through the skin is less than 1/4 inch. The LASE endoscope allows your doctor to see the bulging disc tissue and remove it with the laser fiber. By removing some of the nucleus from the disc, the pressure on the nerve is reduced or eliminated along with the pain.
LASE -bridges the gap between conservative therapy and surgery for the treatment of contained herniated discs. The LASE procedure is a cost-effective, minimally-invasive treatment for those patients who prefer to avoid conventional back surgery. LASE often provides relief from the pain and a fast return to routine activities. Because it is minimally-invasive, it is appropriate for many patients whose health or age may exclude them from more aggressive surgical intervention.