A fusiform aneurysm is a type of aneurysm characterized by a spindle-like shape when viewed in cross-section. Fusiform (“spindle-shaped”) aneurysms are variable in both their diameter and length; their diameters can extend up to 20 cm (8 in). They often involve large portions of the ascending and transverse aortic arch, the abdominal aorta, or less frequently the iliac arteries. The shape of an aneurysm is not pathognomonic for a specific disease. It can be a cause for concern, depending on where in the body it is located, and in some cases emergency surgery may be required to correct it before it ruptures. Rupture of an aneurysm can have fatal consequences; for example, an abdominal aortic aneurysm (AAA) can rupture and cause a patient to bleed to death within minutes.
 Aneurysms are swellings which occur in the vascular system. While some dilation of a vein or artery may not be a major issue, if it dilates enough, the tissue becomes weakened. This means that rupture of the blood vessel is possible, which would cause internal bleeding. Aneurysms can also become hiding grounds for clots, which is a definite problem, and they can cause problems with blood pressure. Part of what keeps blood pressure stable is the width of the blood vessels, and when they dilate and stay dilated, the body cannot regulate blood pressure as effectively.
Aneurysms are swellings which occur in the vascular system. While some dilation of a vein or artery may not be a major issue, if it dilates enough, the tissue becomes weakened. This means that rupture of the blood vessel is possible, which would cause internal bleeding. Aneurysms can also become hiding grounds for clots, which is a definite problem, and they can cause problems with blood pressure. Part of what keeps blood pressure stable is the width of the blood vessels, and when they dilate and stay dilated, the body cannot regulate blood pressure as effectively.
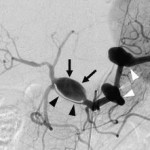
In the case of a fusiform aneurysm, the dilation in the blood vessel looks like a spindle. It is usually a complication of severe atherosclerosis, and is sometimes called an atherosclerotic aneurysm for this reason. Because of the elongated and tortuous shapes of fusiform aneurysms, “dolichoectasia” is another term that has been used to describe them. Diagnosis is performed with the assistance of medical imaging studies, which may include the use of contrast to clearly highlight the vascular system so that abnormalities can be clearly seen on the study.
The initial event in the formation of fusiform aneurysm is thought to be lipid deposition in and beneath the intima that disrupts the internal elastic membrane and infiltrates the muscular wall. The resultant atrophy of the elastic substance and the musculature then leads to tortuosity of the vessel due to intravascular pressure, causing the ectatic vessel to expand in diameter and length.
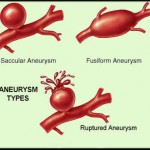
Unlike the focal outpouchings found in saccular aneurysms, in fusiform aneurysms the entire vessel expands, which supports the observation that deficiency of the muscular wall and internal elastic lamina is diffuse. The circulation slows because of this increased luminal diameter, and the resulting turbulent blood flow predisposes the vessel to thrombosis, which promotes further intimal disruption and vessel distortion. Repeated thrombosis near the wall makes the vessel stiff and thick. The natural tendency then for a fusiform aneurysm is to expand and produce mass effects on nearby structures. Or, the expanding fusiform aneurysm can distort vascular branches, reducing distal flow, or can even serve as a nidus for clot formation and distant embolization.
The risk of rupture of the fusiform aneurysm and hemorrhage is reduced due to the diffusely thickened and stiff wall.
If a fusiform aneurysm is small and not in a dangerous location, a doctor may recommend taking a wait and see approach. The aneurysm will be monitored for signs of changes, and the patient may be advised to take some precautionary steps to avoid exacerbation of the aneurysm. If the aneurysm is large, surgical measures may be recommended to address it before it ruptures. Surgery may also be necessary if the aneurysm is in a delicate location where rupture could become an issue.
Symptoms of a fusiform aneurysm vary. Their mass can compress surrounding structures, such as the brain stem. Any fibrofatty thrombus that they contain can fracture, flow through the circulation to other regions of the brain, and cause a stroke. Often, the issue is not identified in the early stages, with problems emerging when the aneurysm is close to rupture and the patient is experiencing symptoms associated with low blood pressure such as dizziness, fainting, and pale skin. The aneurysm may also be identified during medical imaging or routine screening for another medical issue. On imaging scans, these lesions appear as long, wide, serpentine shaped aneurysms.
Once these aneurysms become large, they are notoriously difficult to treat. In their early stages, that is as smaller fusiform aneurysms are symptomatic, for example causing stroke-like factors. This process can involve improving diet and exercise, using medications to lower blood thinner or anti-clotting medication. Open surgical and endovascular options are reserved for such aneurysms that are unresponsive to medical treatments. These options are frequently high-risk. Treatment may involve some form of trapping the aneurysm or sacrificing its parent vessel, with or without an open surgical brain bypass graft. A brain bypass is similar to a heart bypass, where another vessel is harvested by the surgeon and sewn into place, to allow blood to pass by the diseased segment. Surgery for a fusiform aneurysm is performed by a cardiovascular surgeon who works on the patient while she or he is under general anesthesia. The risks of the procedure vary, depending on the location and size of the aneurysm.