Tetralogy of Fallot is a type of congenital heart defect. Congenital means that it is present at birth.
Causes, incidence, and risk factors
Tetralogy of Fallot causes low oxygen levels in the blood. This leads to cyanosis (a bluish-purple color to the skin).
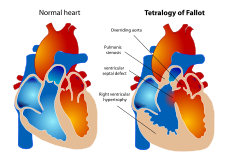
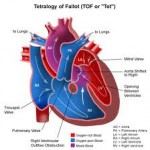
The classic form includes four defects of the heart and its major blood vessels:
- Ventricular septal defect (hole between the right and left ventricles)
- Narrowing of the pulmonary outflow tract (the valve and artery that connect the heart with the lungs)
- Overriding aorta (the artery that carries oxygen-rich blood to the body) that is shifted over the right ventricle and ventricular septal defect, instead of coming out only from the left ventricle
- Thickened wall of the right ventricle (right ventricular hypertrophy)
 Tetralogy of Fallot is rare, but it is the most common form of cyanotic congenital heart disease. Patients with tetraology of Fallot are more likely to also have other congenital defects.
Tetralogy of Fallot is rare, but it is the most common form of cyanotic congenital heart disease. Patients with tetraology of Fallot are more likely to also have other congenital defects.
The cause of most congenital heart defects is unknown. Many factors seem to be involved.
Factors that increase the risk for this condition during pregnancy include:
- Alcoholism in the mother
- Diabetes
- Mother who is over 40 years old
- Poor nutrition during pregnancy
- Rubella or other viral illnesses during pregnancy
Children with tetralogy of Fallot are more likely to have chromosome disorders, such as Down syndrome and DiGeorge syndrome (a condition that causes heart defects, low calcium levels, and poor immune function).
Specific genetic associations include:
- JAG1
- NKX2-5
- ZFPM2
- VEGF
Symptoms
- Blue color to the skin (cyanosis), which gets worse when the baby is upset
- Clubbing of fingers (skin or bone enlargement around the fingernails)
- Difficulty feeding (poor feeding habits)
- Failure to gain weight
- Passing out
- Poor development
- Squatting during episodes of cyanosis
Signs and tests
A physical examination with a stethoscope almost always reveals a heart murmur.
Tests may include:
- Chest x-ray
- Complete blood count (CBC)
- Echocardiogram
- Electrocardiogram (EKG)
- MRI of the heart (generally after surgery)
Pathophysiology
Primary four malformations
 “Tetralogy” denotes a four-part phenomenon in various fields, including literature, and the four parts the syndrome’s name implies are its four signs. This is not to be confused with the similarly named teratology, a field of medicine concerned with abnormal development and congenital malformations, which thereby includes tetralogy of Fallot as part of its subject matter.
“Tetralogy” denotes a four-part phenomenon in various fields, including literature, and the four parts the syndrome’s name implies are its four signs. This is not to be confused with the similarly named teratology, a field of medicine concerned with abnormal development and congenital malformations, which thereby includes tetralogy of Fallot as part of its subject matter.
As such, by definition, tetralogy of Fallot involves exactly four heart malformations which present together:
|
Condition |
Description |
| A: Pulmonary Infundibular Stenosis | A narrowing of the right ventricular outflow tract. It can occur at the pulmonary valve (valvular stenosis) or just below the pulmonary valve (infundibular stenosis). Infundibular pulmonic stenosis is mostly caused by overgrowth of the heart muscle wall (hypertrophy of the septoparietal trabeculae), however the events leading to the formation of the overriding aorta are also believed to be a cause. The pulmonic stenosis is the major cause of the malformations, with the other associated malformations acting as compensatory mechanisms to the pulmonic stenosis. The degree of stenosis varies between individuals with TOF, and is the primary determinant of symptoms and severity. This malformation is infrequently described as sub-pulmonary stenosis or subpulmonary obstruction. |
| B: Overriding aorta | An aortic valve with biventricular connection, that is, it is situated above the ventricular septal defect and connected to both the right and the left ventricle. The degree to which the aorta is attached to the right ventricle is referred to as its degree of “override.” The aortic root can be displaced toward the front (anteriorly) or directly above the septal defect, but it is always abnormally located to the right of the root of the pulmonary artery. The degree of override is quite variable, with  5-95% of the valve being connected to the right ventricle. |
| C: ventricular septal defect (VSD) | A hole between the two bottom chambers (ventricles) of the heart. The defect is centered around the most superior aspect of the ventricular septum (the outlet septum), and in the majority of cases is single and large. In some cases thickening of the septum (septal hypertrophy) can narrow the margins of the defect. |
| D: Right ventricular hypertrophy | The right ventricle is more muscular than normal, causing a characteristic boot-shaped (coeur-en-sabot) appearance as seen by  chest X-ray. Due to the misarrangement of the external ventricular septum, the right ventricular wall increases in size to deal with the increased obstruction to the right outflow tract. This feature is now generally agreed  to be a secondary anomaly, as the level of hypertrophy generally increases with age. |
There is anatomic variation between the hearts of individuals with tetralogy of Fallot. Primarily, the degree of right ventricular outflow tract obstruction varies between patients and generally determines clinical symptoms and disease progression.
Treatment
 Surgery to repair tetralogy of Fallot is done when the infant is very young. Sometimes more than one surgery is needed. When more than one surgery is used, the first surgery is done to help increase blood flow to the lungs.
Surgery to repair tetralogy of Fallot is done when the infant is very young. Sometimes more than one surgery is needed. When more than one surgery is used, the first surgery is done to help increase blood flow to the lungs.
Surgery to correct the problem may be done at a later time. Often only one corrective surgery is performed in the first few months of life. Corrective surgery is done to widen part of the narrowed pulmonary tract and close the ventricular septal defect.
Expectations (prognosis)
Most cases can be corrected with surgery. Babies who have surgery usually do well. More than 90% survive to adulthood and live active, healthy, and productive lives. Without surgery, death usually occurs by the time the person reaches age 20.
Patients who have continued, severe leakiness of the pulmonary valve may need to have the valve replaced.
Regular follow-up with a cardiologist to monitor for life-threatening irregular heart rhythms (arrhythmias) is recommended.
Complications
- Delayed growth and development
- Irregular heart rhythms (arrhythmias)
- Seizures during periods when there is not enough oxygen
- Death
Calling your health care provider
Call your health care provider if new unexplained symptoms develop or the patient is having an episode of cyanosis (blue skin).
If a child with tetralogy of Fallot becomes blue, immediately place the child on his or her side or back and put the knees up to the chest. Calm the baby and seek medical attention immediately.
